We are proud to announce that Custom Software Lab has helped Apollo Practice Management to introduce customized SOAP notes module in record time.
SOAP notes ensure that your practice workflow runs smoothly while ensuring that you do not miss a beat with your patients. Standing for Subjective, Objective, Assessment, and Plan, SOAP is a template that ensures service providers systematically capture patient notes during the course of treatment.
Documentation is a critical component of patient care. Having access to accurate and precise information at every step of patient care improves overall health care and patient experience. Apollo Practice Management makes it easy for health providers to document a patient’s treatment progress using SOAP notes digitally.
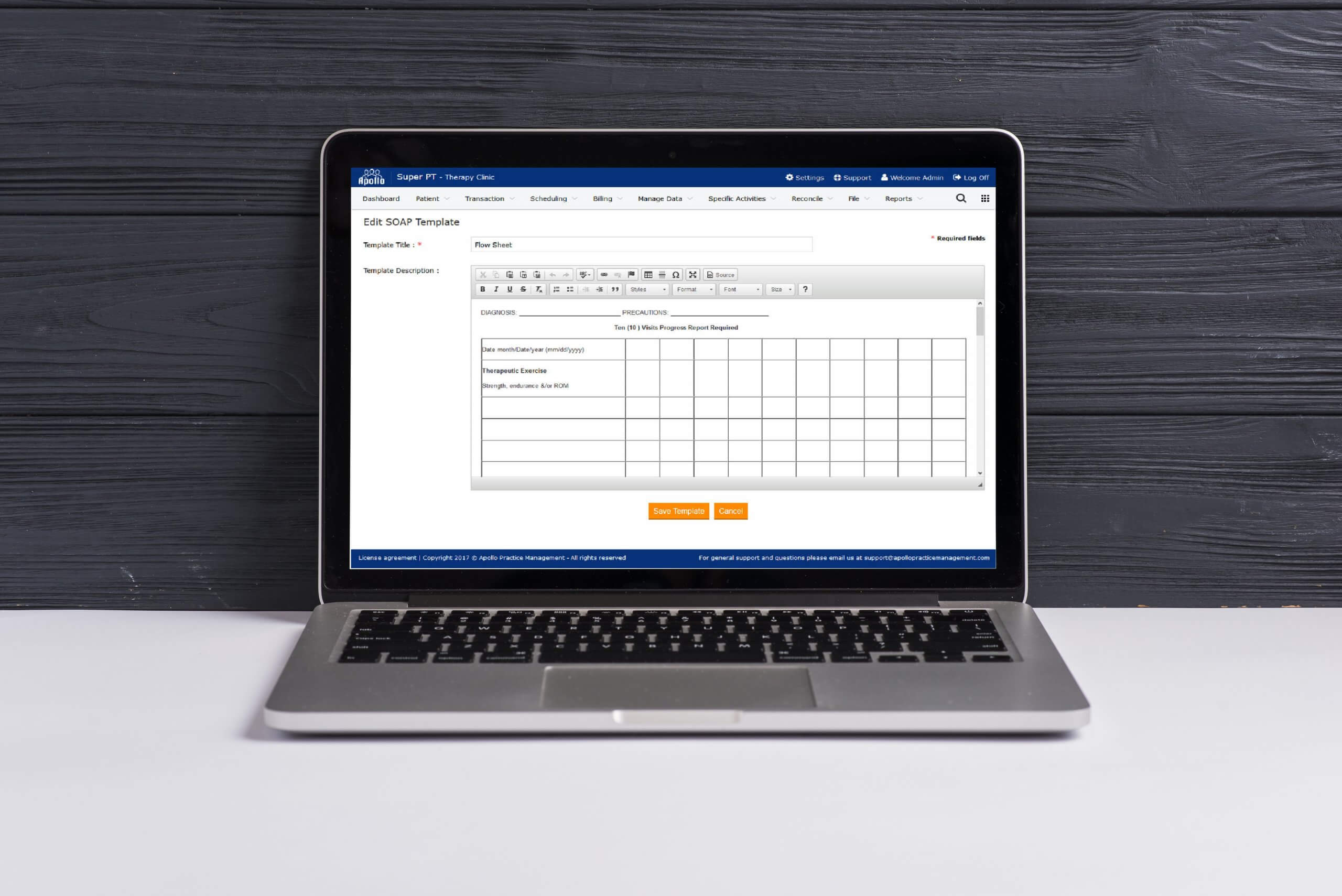
Custom Software Lab has helped to design a new generation of SOAP notes that tightly integrates with PT’s practice and give a seamless experience between clients, appointments, staff members, chart notes, and patient files. The updated version enables PTs to harness the power of technology to write comprehensive SOAP notes quickly and efficiently.
The newly launched customized SOAP notes help PTs for full customization of SOAP notes to match their treatment style, different types of patients, or even their working site – whatever helps them to stay organized. PTs can now create forms, sections, notes, and add comments as per their needs with the least possible efforts and significantly reduced chance of error.
Adding information is a time-consuming task that can lengthen the patient wait times and often put a wrench in their day. With the many tasks, clinical staff must do throughout the day, it becomes imperative to make your Initial Evaluation note flow more quickly and concise. With the new version of SOAP notes, the staff can take all the tests and forms and put them in a category (of your choosing) under ‘Objective.’ This will now streamline the Initial Evaluation, which will enable the clinician to spend less time taking the notes and more time with the patient.
A customized SOAP template means having a unique template built specifically for your practice that is flexible and can be altered to adhere to any unique needs of your practice. PTs can set up their own forms using custom fields to enable staff to enter data quickly and efficiently. With mobile support for SOAP Notes, therapists can enter and access notes directly from a tablet, a smartphone or computer.
Possibly one of the most notable benefits of having a customizable SOAP template is the elasticity that customized documenting provides. It helps the provider to bypass the repetitive frustrations of documentation while ensuring that all of your patient’s interactions and health information is stored in a single, convenient location. Having a customizable SOAP template will give your practice the freedom to practice medicine its own way. It works to take the stress away and puts you back in the exam room.
Our team, armed with years of experience in working with PT software – Apollo Practice Management, promptly recognized the need to adopt the custom features that catered to the unique needs of PTs operations and helped launch the new version in record time.
